Chronic back and neck pain can be debilitating, affecting your daily life and overall well-being. If you’ve tried various treatments with little success, medial branch nerve radiofrequency ablation, also known as medial branch RF thermocoagulation or facet joint denervation, might be the solution you’ve been searching for. In this article, we’ll delve into what this procedure entails, who it’s suitable for, and what you can expect during and after the process.
The spine is made up of vertebrae, and between these vertebrae, there are facet joints that provide stability and allow for various types of spinal movements. These facet joints are rich in nerve endings, which are responsible for transmitting pain signals when the joints are irritated or inflamed. The medial branch nerves are small nerve branches that innervate the facet joints, serving as pain messengers.

Radiofrequency denervation is a procedure that uses radiofrequency to desensitize the nerve responsible for the pain, rendering it incapable of sending pain signals on a permanent basis. Medial branch nerve radiofrequency (RF) ablation, is a minimally invasive medical procedure aimed at alleviating chronic pain in the neck and back, primarily caused by issues related to the facet joints in the spine. This procedure specifically targets the medial branch nerves, which play a crucial role in transmitting pain signals from the facet joints to the brain.
Medial branch nerve RF ablation is recommended for people with chronic neck or back pain, typically associated with facet joint disorders. Common conditions that may benefit from this procedure include:
Facet joint osteoarthritis: When the joints in the spine become inflamed or degenerate, they can cause severe pain in the back and neck.
Spondylosis: This is a degenerative condition that affects the discs and facet joints of the spine, causing pain and stiffness.
Whiplash injuries: In some cases, patients with unresolved whiplash injuries can develop chronic neck pain that can be treated with this procedure.
Although medial branch nerve RF ablation is effective for many patients, it may not be suitable for everyone. Contraindications include:
Pregnancy: It is not recommended for pregnant women due to potential risks to the unborn child.
Infection at the treatment site: If you have an infection at the site of the procedure, it’s important that it’s treated before you undergo this procedure.
Allergic reactions: Some people may be allergic to the materials used in the procedure.
Bleeding disorders: Patients with bleeding disorders or those taking anticoagulant medications that interfere with blood clotting may not be suitable candidates for medial branch RF thermocoagulation.
Before undergoing medial branch nerve radiofrequency denervation, patients often undergo a diagnostic phase to confirm the source of their pain. This phase usually consists of the following steps:
Initial assessment: Your healthcare provider will thoroughly review your medical history, perform a physical examination and review any previous imaging studies.
Imaging studies: X-rays, MRI or CT scans may be ordered to help determine the exact location of the source of pain, especially the facet joints in the spine.
Medial branch nerve block: A medial branch nerve block is used to confirm that the pain is coming from the medial branch nerves.
After the diagnostic medial branch nerve blocks, you will be observed for a short period to assess the degree of pain relief. If the diagnostic blocks provide significant relief (more than 50%), you may be considered a suitable candidate for the next stage, which is medial branch radiofrequency denervation.
Once you’ve been determined to be a candidate for the procedure, your physician will give you pre-procedure instructions. This will usually include instructions on fasting before the procedure, stopping certain medications (such as blood thinners), and arranging transportation to and from the medical facility.
You will have a peripheral vascular line inserted before the procedure and vital signs such as pulse rate, blood oxygen level and arterial blood pressure will be monitored once you are in the procedure room.
Before the procedure begins, you’ll be positioned on the procedure table to allow access to the target area. Your healthcare provider will ensure that you are comfortable for the procedure and that you are positioned appropriately in the prone position. Specific positioning may vary depending on whether the medial branch nerve being treated is in the lumbar (lower back) or cervical (neck) region.
After proper positioning, a local anaesthetic is administered to numb the specific area to be treated. This local anaesthetic helps to minimise any pain or discomfort during the procedure. In some cases, conscious sedation may also be used to help you relax and feel more comfortable.
After the anaesthetic and sedation have taken effect, a small, specialised RF needle is carefully guided to the medial branch nerve under fluoroscopic guidance. The aim is to place the needle close to the nerve while avoiding vital structures. After the needle is placed in the right place fluoroscopically, motor and sensory stimuli are given. Small adjustments can be made to be in the closest position to the medial branch nerve.
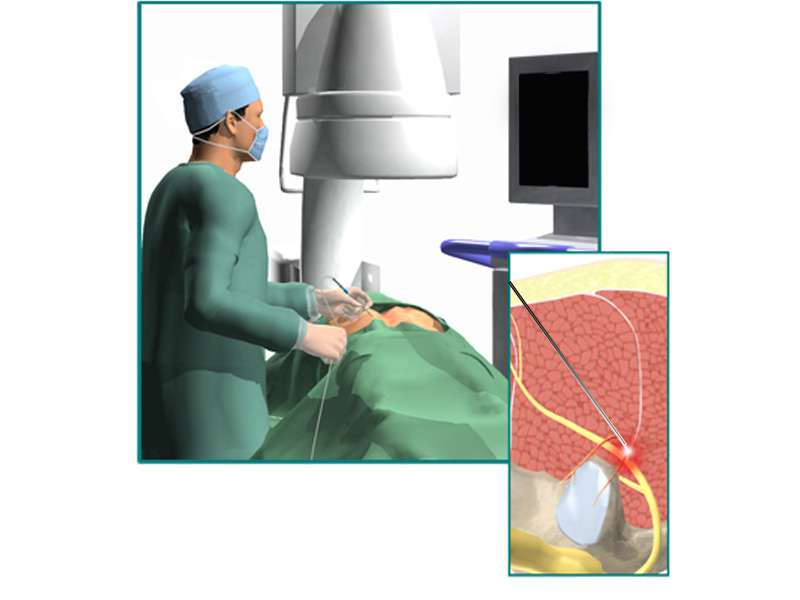
Once the needle is in the correct position, the radiofrequency (RF) ablation procedure begins. RF generates high-frequency electrical currents that heat the tip of the needle. This heat is delivered precisely to the nerve, causing it to coagulate, or essentially ‘burn’, and disrupting its ability to transmit pain signals. The temperatures used are carefully controlled to avoid excessive damage to surrounding tissue.
After the RF thermocoagulation procedure, you will be kept under observation for a short time to monitor your immediate post-procedure condition. This is to ensure that there are no complications and that your vital signs are stable. It’s common for patients to experience mild discomfort or soreness at the treatment site during this time.
You’ll usually spend a short time in a recovery room where the effects of sedation or anaesthesia wear off. Your healthcare provider will give you post-operative care instructions, which may include recommendations for rest, over-the-counter pain relief, and any activity restrictions. It’s important to follow these instructions to ensure a smooth recovery.
Complications associated with medial branch nerve RF ablation are rare, but they can occur. The following are some of the potential complications that can occur with this procedure:
Infection: Infection is a risk common to all invasive procedures, including medial branch nerve denervation.
Bleeding: Bleeding is a rare complication, but is more common in patients with underlying bleeding disorders.
Allergic reaction: A potential allergy is usually to the X-ray contrast agent and rarely to the local anaesthetic.
Aggravation of pain symptoms: In rare cases, patients may experience an increase in pain symptoms after the procedure.
Discomfort at the injection site: Patients may experience some discomfort or soreness at the injection site, but this usually resolves within a few days.
Nerve or spinal cord damage or paralysis: Although very rare, damage can occur as a result of direct trauma from the needle, or secondarily from infection, bleeding causing compression, or injection into an artery causing blockage.
In the days and weeks following your procedure, you’ll have a follow-up appointment with your physician. During this visit, your pain relief will be assessed and any necessary adjustments or additional treatments may be discussed.
Keep in mind that the specific details of each procedure may vary depending on the healthcare facility, the healthcare provider’s practices, and individual patient needs. Always consult with your healthcare provider for personalised information and guidance regarding medial branch RF denervation.