Tension-Type Headache: Symptoms, Diagnosis and Treatment Options
Headaches are a common condition that affects millions of people worldwide, disrupting daily life and productivity. Among the different types of headache, tension-type headache is one of the most common. Tension-type headache (TTH) is a common neurological condition characterised by recurrent episodes of mild to moderate headache lasting minutes to weeks. It is the most common neurological disorder worldwide, affecting up to 78% of headache sufferers in population-based studies. This type of headache used to be known by many terms, such as stress headache, psychomyogenic headache, muscle contraction headache, etc.
However, the term “tension-type headache” (TTH) was adopted by the International Classification of Headache Disorders I in 1988 and retained by ICHD II in 2004. TTH is the least well defined of all headache types and its pathogenesis is uncertain. The adjectives “tension” and “type” emphasise its unclear pathogenesis and suggest that some form of mental or muscular tension may play a causative role. However, a large number of clinical and neurophysiological studies leave little doubt about its classification and nomenclature.
What is a tension-type headache?
Tension-type headache, often referred to as TTH, is a primary type of headache characterised by a dull, aching pain that can spread across the forehead, temples and back of the head. They are typically described as a tight band or pressure around the head that causes discomfort. Unlike migraines, tension-type headaches are not usually accompanied by blurred vision, nausea or vomiting.

Symptoms of tension-type headache
Tension-type headaches can vary in intensity and duration, but they are often accompanied by the following symptoms:
- Aching pain: The hallmark of a tension-type headache is a constant, aching pain that affects both sides of the head. This pain is often described as a constant, mild to moderate pressure.
- Duration: Tension-type headaches can last from 30 minutes to several days. Some people have chronic tension-type headaches, which occur 15 or more days a month for at least three months.
- Location: The pain is usually felt in the forehead, temples and back of the head or neck. It may radiate to the shoulders and upper back.
- Tightness: Many people with tension-type headaches report a feeling of tightness or a “band” of pressure around the head.
- Sensitivity to light and noise: Although not as pronounced as in migraines, some people with tension-type headaches may still be sensitive to light (photophobia) and sound (phonophobia).
How tension-type headache is diagnosed
To diagnose tension-type headache and rule out other possible causes, healthcare providers often follow these steps
Medical history: The first step is a thorough discussion of your medical history and headache symptoms. Be prepared to provide details about the frequency, duration, and intensity of your headaches.
Physical examination: A physical examination may be performed to look for signs of underlying medical conditions that may be contributing to the headache.
Diagnostic criteria: Tension-type headache is usually diagnosed according to the diagnostic criteria of the International Classification of Headache Disorders (ICHD).
Imaging tests: In some cases, if there are atypical symptoms or neurological concerns, your doctor may order imaging tests such as MRI or CT scans to rule out other causes.
Treatment options for tension-type headaches
Fortunately, there are several treatment options available, ranging from lifestyle changes to medical interventions. Here’s an overview:
Over-the-counter pain relievers
Simple analgesics: Medications such as acetaminophen (Tylenol) and non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin) or aspirin are often the first line of treatment. These medicines can be effective in relieving the pain associated with tension-type headaches.
Caution: It’s important to use these medications as directed to avoid overuse, which can lead to medication-overuse headache or other side effects.
Prescription medications
Muscle relaxants: In some cases, especially when over-the-counter options are ineffective, doctors may prescribe muscle relaxants. These can help relieve the muscle tension that contributes to these headaches.
Other prescription medications: For chronic tension-type headaches, your doctor may suggest other types of prescription medications, such as antidepressants or anti-anxiety medications. These are usually considered if the headaches are frequent or severe.
Interventional treatments for tension-type headaches
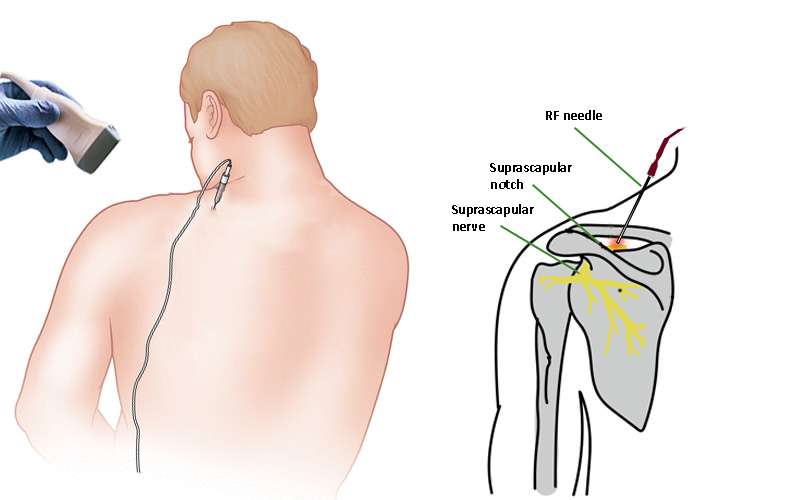
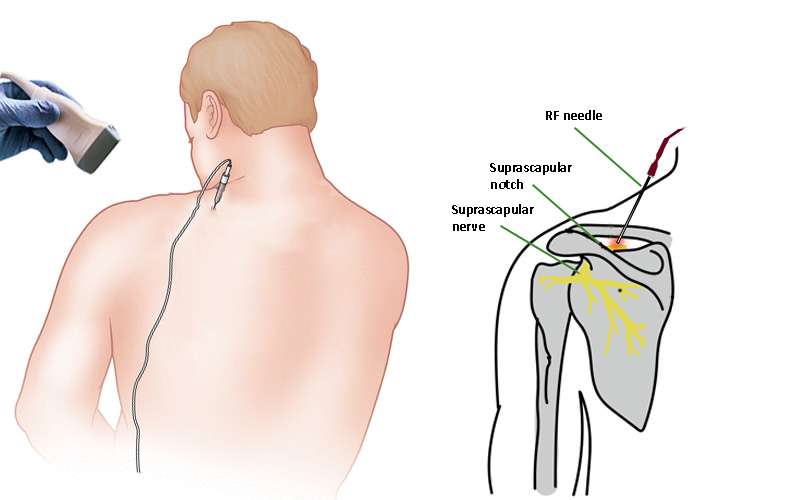
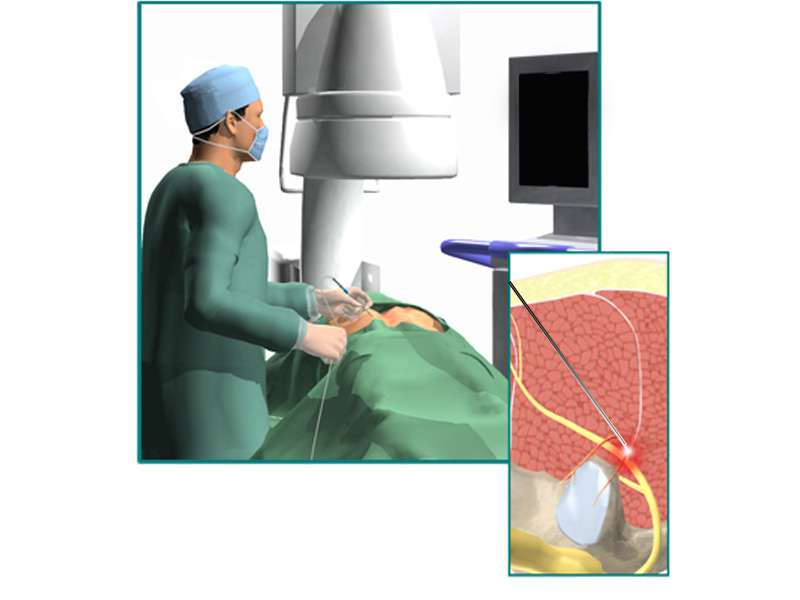
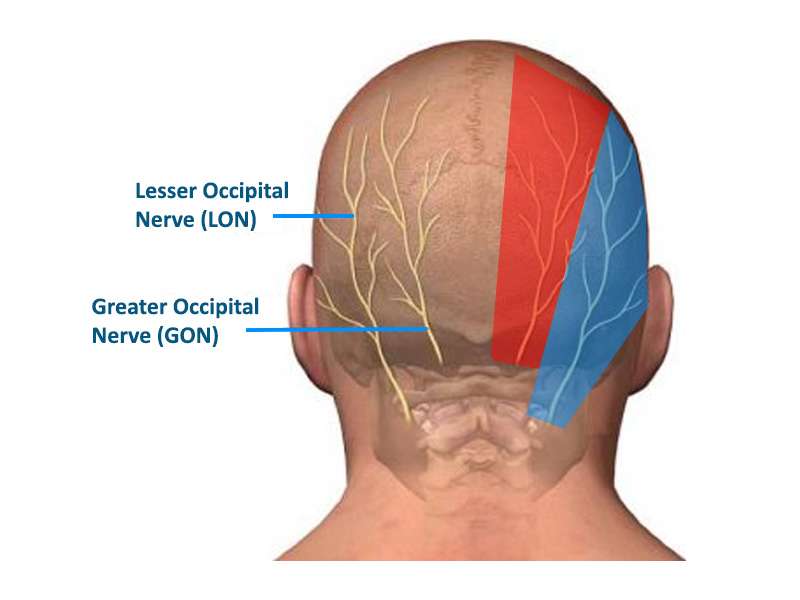
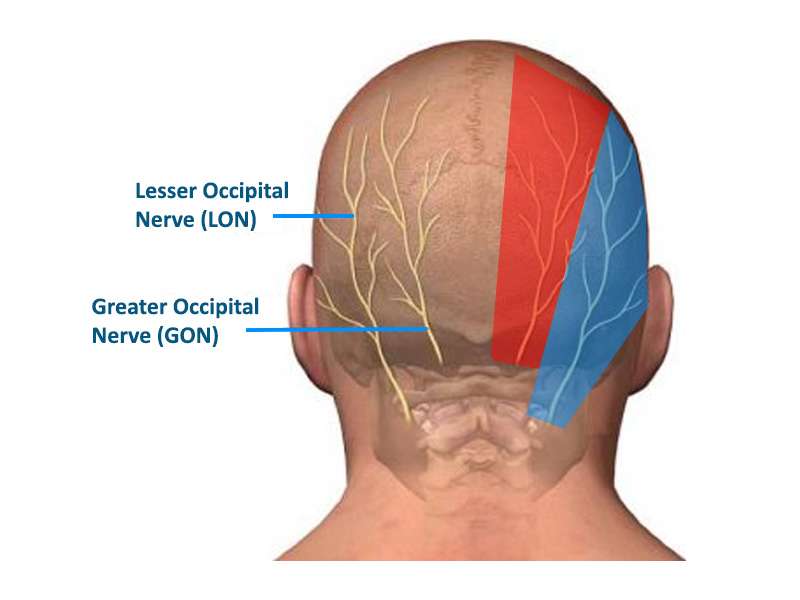
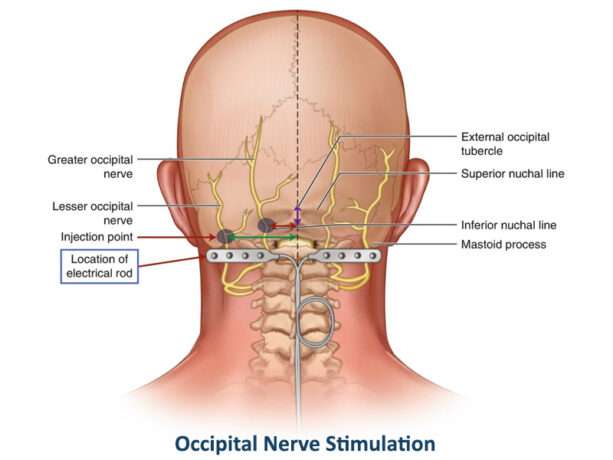
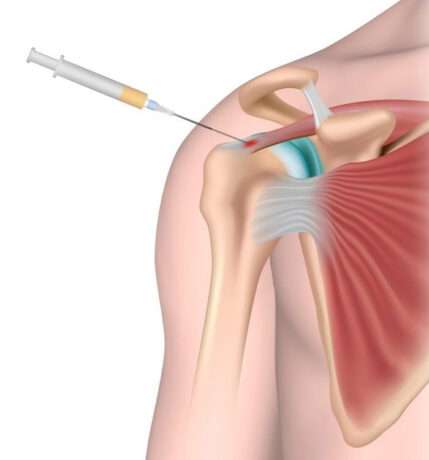
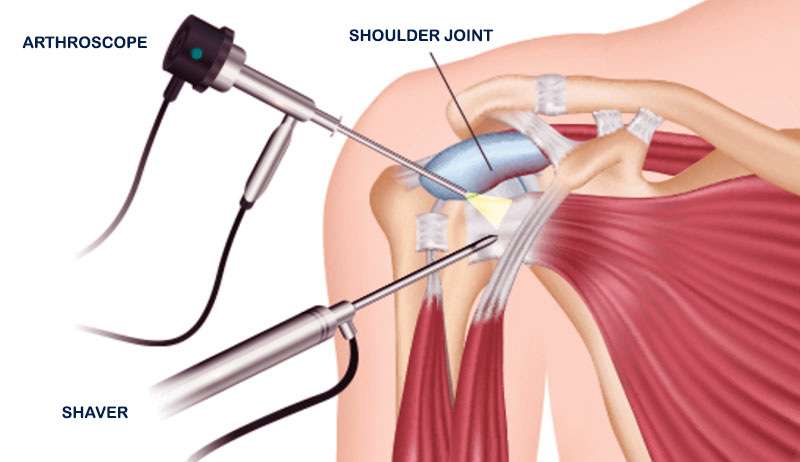
For people with chronic tension-type headaches for whom conventional treatments have limited effectiveness, interventional treatments may offer relief. These advanced methods focus on targeting the specific pain pathways involved in headaches. One such technique is nerve block injections, where anaesthetics are injected into specific nerves (such as the occipital nerves) to provide pain relief. Another option is trigger point injections, where pain-relieving medication is injected into specific areas of muscle tension or ‘trigger points’ that are thought to be the source of the headache. It’s important to note that these interventional treatments should only be considered under the guidance of a healthcare professional who specialises in pain management. They will assess the individual’s specific condition, determine the suitability of these approaches and ensure that they are carried out safely and effectively.
Lifestyle changes
Stress management: Learning stress-reduction techniques such as deep breathing, progressive muscle relaxation, meditation or yoga can help relieve stress-induced tension-type headaches. Regular practice of these techniques can improve your ability to cope with stressful situations.
Regular exercise: Regular physical activity can help reduce the frequency and severity of tension-type headaches. Aim for at least 30 minutes of moderate exercise most days of the week.
Sleep hygiene: Make sure you get enough restful sleep by keeping a consistent sleep schedule, creating a comfortable sleeping environment, and avoiding caffeine or stimulating activities close to bedtime.
Biofeedback and physiotherapy
These therapies can help you learn to control muscle tension, a common trigger for tension-type headaches. Biofeedback involves monitoring and regulating physiological responses, while physical therapy focuses on exercises and techniques to improve posture and reduce muscle tension.
Alternative therapies
Acupuncture: Some people find relief from tension-type headaches through acupuncture, a traditional Chinese medicine practice that involves inserting thin needles into specific points on the body.
Chiropractic care: Chiropractic adjustments can help relieve tension in the neck and shoulders, potentially reducing the frequency and intensity of headaches.
Herbal supplements: Certain herbal remedies, such as feverfew and butterbur, have been studied for their potential to prevent headaches. Consult your healthcare professional before trying any herbal supplements.
Trigger avoidance
Identify and avoid specific triggers that may contribute to your tension-type headaches. Common triggers include certain foods (e.g. caffeine, aged cheeses), alcohol and environmental factors (e.g. bright lights, loud noises).
Keep a headache diary to keep track of potential triggers and patterns so you can better manage and avoid them.
In summary, tension-type headaches are a common and often distressing condition, but there are several treatment options available to help manage and relieve the pain associated with them. It’s important to work with a healthcare professional to determine the most appropriate treatment plan for your particular condition. By taking a multifaceted approach that includes lifestyle changes, self-care strategies and, if necessary, medications or alternative therapies, you can take steps to minimise the impact of tension-type headaches on your daily life. Remember that consistent self-care and regular communication with your healthcare provider are key to effectively managing this common condition and improving your overall quality of life.